Current Issues
Case Report
Endoscopic repair of CSF leak
*Corresponding Author
P Venu Gopal Reddy
Assistant Professor, Department of Ear, Nose and Throat,
Kamineni Institute of Medical Sciences, Narketpally, Nalgonda district, Telangana State, India - 508254.
Email:p.venugopalreddy1985@gmail.com
Assistant professorl,Post graduate2 ,Professor3,Professor & Head4, Department of Ear, Nose and Throat, Kamineni Institute of Medical Sciences, Narketpally, Nalgonda, Telangana State, India.
Abstract
A case of 40 yrs old female with spontaneous CSF rhinorrhea on left side for 2 months. After confirming the diagnosis and treating the patient for lowering of raised intracranial pressure, endoscopic repair done through Transnasal approach by onlay technique using mucosa of middle turbinate, middle turbinate with pedicle as graft materials.
Key Words: CSF rhinorrhoea, endoscopy
Introduction
Cerebrospinal fluid (CSF) rhinorrhea involves a communication between the subarachnoid space and the nose. The etiologic classification of CSF leak was developed by Ommaya et al.6 He classified CSF rhinorrhoea into 1)Traumatic 2) Non-traumatic or spontaneous. Non-traumatic again subdivided into a) Primary - where no underlying cause can be found b) Secondary - intracranial pathology (high or normal pressure). High pressure leaks include tumours, benign intracranial hypertention and hydrocephalus. Normal pressure leaks are due to empty sella syndrome, tumours, congenital defects, infection, arachnoid granulations, meningoencephaloceles and idiopathic.Majority of spontaneous cases occur in adults in fourth decade of life with females out numbering males (2:1).
Non-traumatic leaks are less common, insidious in onset and often mistaken for a symptoms of rhinitis. The site of fistulous communication in spontaneous CSF leak involves the dehiscence in the cribriform plate, fovea ethmoidalis, sphenoid sinus and rarely the frontal sinus. Meningitis, the main danger in traumatic cases is much less common in the non traumatic patients. Traditionally spontaneous CSF leaks have been managed by the neurosurgeons via a frontal craniotomy with the success rate between 60 and 80%. It has been associated with significant conditions such as frontal lobe retraction and anosmia. Wigand (1981) and Stankiewicz (1987) were the first to describe the transnasal endoscopic closure. In recent years it has gained popularity and is now considered to be the treatment of choice for CSF rhinorrhea. Endoscopic transnasal approach has a success rate of between 76% and 95%.
Case Report

Fig 1: Watery nasal discharge seen on bending forward

Fig 2: Endoscopic view of meninges prolapsing in nasal cavity
A 40 years old female patient admitted with history of clear watery nasal discharge from left side of nose since 2 months, the watery nasal discharge was observed when the patient bends forward (Fig. 1).
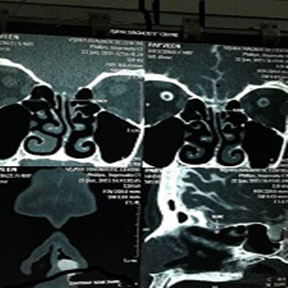
Fig 3: CT cisternography showing CSF leak

Fig 4: Underlay technique
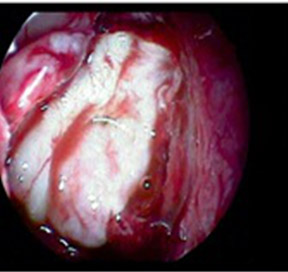
Fig 5: Graft supported with surgicel
There was no previous history of accidental or Iatrogenic trauma or history of meningitis. She is a known case of diabetes and hypothyroidism and on medications. On examination she had deflected nasal septum towards right side and other E.N.T examination findings were within normal limits. Diabetic profile and thyroid profile were within normal limits. A CT Cisternography of Paranasal sinus was done (Fig. 3). The clear fluid collected on stooping was sent for glucose analysis (61mg/dl) and was suggestive of CSF.
Prophylactic antibiotics were given to prevent meningitis. Intravenous mannitol twice daily and tablet acetazolamide 250mg three times daily (8th hourly) was given to control intracranial pressure. As there was no response for medical treatment, surgical repair was planned. The surgery was done under general anaesthesia. The nasal cavity was packed with 4% xylocaine and 1:200000 adrenaline. After infiltration, antero-inferior part of middle turbinate was harvested as pedicle graft. Site of leak identified with endoscope, mucosalflap of middle turbinate placed over the defect by underlay technique (Fig. 4). Harvested middle turbinate with pedicle is rotated to snugly fit in between the well placed mucosal flap, skull base and the remnant middle turbinate. The repaired area was supported with surgicel. The nasal packing was done with antibiotic soaked ribbon gauze. Nasal pack was removed after 48 hrs. Follow up after one month showed no evidence of recurrence.
Discussion
Majority of CSF leaks presented are unilateral. Clear nasal discharge has been tested historically for glucose but is not diagnostic of CSF leak. False positive s occur due to the presence of lacrimal and nasal reducing substances. However, absence of glucose rules out CSF rhinorrhea. Beta-2 transferrin has become a diagnostic test for CSF fistula with a nearing 100% and specificity of 95%. It is a protein found only in CSF, aqueous humor and perilymph. Precise preoperative localization of CSF leak is essential for surgical repair. The main problem of imaging modalities relates to the fact that spontaneous CSF leak may not be actively leaking at the time of the investigation. High resolution CT scans have been advocated as the non-invasive radiological investigation of choice. The sensitivity rate has been reported from 50 to 100%. However, the main drawbacks are its high radiation to the lens and the bony defect may not correspond to the site of dural tear. In the presence of frequent or constant CSF rhinorrhea, a CT cisternography can be helpful in defining the exact site of leak. The overall accuracy improves from 40 to 92% if the leak is active. The disadvantages of CT cisternography is, it is invasive, time consuming requiring a lumbar puncture and intrathecal injection of contrast. Advantages of endoscopic repair includes 1)Excellent visualization 2)Precise graft placement 3)Shortened operating time 4)Minimizes intranasal trauma and preserves the bony framework supporting the frontal recess and other critical areas. There have been numerous reports describing various grafting techniques employed in endoscopic repair of CSF leak. The choice of the materials and techniques used during the endoscopic procedure depends on the experience and familiarity of the surgeon with various techniques. Weber et al (1996) used both free grafts and vascularised flaps with onlay and underlay techniques and successfully repaired all his 42 patients. Wormald and McDonough5 presented the 'bath plug' technique, which consisted of introducing a fat plug with vicryl suture into the intradural space in which the dural defects was less than 15mm. They claim that this technique would prevent high pressure from pushing the graft away from the defect. valsalva maneuvers were performed to ensure the stability of the graft intraoperatively. The size of the defect dictates the type of material used in the repair. Larger defect (usually more than 3cm) may require bone or cartilage in addition to soft tissue.Patients are instructed to refrain from strenous activity for 2 to 4 weeks. Avoidance of sneezing or coughing, use of stool softners, elevation of the head and bedrest are essential to give the graft time to heal. Close follow up is important to evaluate the success of the repair.
Conclusion
Endoscopic repair of CSF rhinorrhoea provides a better field of vision with enhanced illumination, magnified angle of visualization and accurate positioning of the graft under direct visualization. The high success rate attached with this should make it the preferred approach in traumatic and non-traumatic CSF leaks, not associated with intracranial space occupying lesions.
References
- Hughes RG, Jones NS, Robertson I. The endoscopic treatment of cerebrospinal fluid rhinorrhea: The Nottingham experience. J Laryngol Otol 1997; 111: 125-28.
- Mattox D, Kennedy D. Endoscopic management of cerebrospinal Fluid leaks and cephaloceles. Laryngoscope 1990; 100: 857-62.
- Ramsden JD, Rogan Corbridge, Grant Bates. Bilateral 'cerebrospinal fluid rhinorrhea. J Laryngol Otol 2000; 114: 137-38.
- Shetty PG, Shroff M, Sahani DV et al. Evaluation of high resolution CT and MRI cisternography in the diagnosis of cerebrospinal fluid fistula. Am J Neuroradiol 1998; 19: 633-39.
- Wormald P, McDonough M. Bath plug technique for the endoscopic management of cerebrospinal fluid leaks. J Laryngol Otol 1997; 111: 1042-46.508.
- Ommaya AK, Di Chiro et al. Hydrocephalus and leaks. In: Wager H (ed) Principles of nuclear medicine, 2nd edition Phildelphia Saunder 1995.


