CASE RECORD
Case Records in Kamineni Institute of Medical Sciences: High-Altitude Breathlessness Refractory to Descent.
Dr. L. Srujan Reddy,1 Aarti Sahu, 2 Dr. M. Manasa Reddy,3 Dr. Aditya Samitinjay Gade4
1,3,4 Post Graduate, Department of General Medicine, Kamineni Institute of Medical Sciences, Narketpally 2 Undergraduate Medical Student, Department of General Medicine, Kamineni Institute of Medical Sciences, Narketpally
*Corresponding Author
Dr. Aditya Samitinjay GadeDepartment of Internal Medicine,
Kamineni Institute of Medical
Sciences, Narketpally, India - 508284.
Email: adityasamitinjay@outlook.com
Abstract:
This case was presented in Kamineni Institute of Medical sciences on 20th December 2018. Pulmonary Embolism (PE) and High Altitude Pulmonary Edema (HAPE) are different entities which can present with non-specific but similar symptoms and have differing treatment modalities. While HAPE can resolve with increased oxygen supply during descent from high altitude, the diagnosis of PE requires definitive treatment and if missed may result in death. When a patient with HAPE does not improve with descent and oxygen, then other diagnoses must be suspected including PE. PE can co-exist with HAPE or mimic it and should be considered in any patient with shortness of breath in high altitude areas regardless of thrombotic risk factors.
Key words: Pulmonary embolism, High altitude pulmonary edema, thrombosis
Introduction:
This case was presented in Kamineni Institute of Medical Sciences on 20th December 2018. The HAPE incidence among trekkers in the Himalayas and climbers in the Alps ascending at a rate > 600m/day is around 4%.1-3 In an unselected population of Indian soldiers, airlift to an altitude of 5500 m was associated with a HAPE incidence of up to 15%. 4 Immediate improvement of oxygenation either by supplemental oxygen, hyperbaric treatment, or by rapid descent is the treatment of choice for HAPE. 1 But if the symptoms do not improve with treatment then Pulmonary embolism must be suspected and treated to prevent morbidity. Severe pulmonary arterial thrombosis and pulmonary infarcts were noted in autopsies of four out of seven trekkers in the Himalayas 5 with the remaining three noted to have cerebral oedema; two with brain herniation. Approximately 100,000 foreigners trek in Nepal annually (Nepal Tourism statistics 2014). From 2013 to 2015, over 1000 persons were seen at Canadian International Water and Energy Consultants (CIWEC) Clinic at 1400 m with altitude illnesses, including 217 with High Altitude Cerebral Edema (HACE) and 303 with HAPE. Among 303 persons diagnosed with HAPE at initial presentation, 8 were shown to have PE by computed tomography pulmonary angiography (CTPA) and an equal number suspected of having PE had a negative CTPA.(6) This care report hopes to raise awareness of possibility of PE as a differential diagnosis for patients suspected to be having HAPE.
Case Record:
26-year-old man from Haridwar, working as a technician on High Performance Liquid Chromatography (HPLC) in a pharmaceutical research and development company, came with the chief complaints of shortness of breath for 40 days. Swelling in the right limb for 30 days, fever for 30 days blood in stools about 20 days ago. The patient went on a trip from Haridwar (1030 ft) to Dehradun, Srinagar, Kargil, Leh, and Ladhak from 31st July to 6th August 2018. He was apparently asymptomatic till 6th August. When they began the descent on 6th from Ladakh (9800 ft), he started getting breathless. He
was traveling uphill (45-degree angle slope) on a bike as a pillion rider when his shortness of breath increased (Grade 4) and he had to be shifted to a hospital at Keylong (10990 ft). There he was given Acetazolamide, Dexamethasone, Deriphylline. The doctors advised him to shift to a lower altitude so that his symptoms might subside. The patient descended to Manali (6700 ft) on the night of August 6th and stayed there overnight before coming back to Hardiwar on August 9th. On August 9th, he had fever (101°F), shortness of breath persisted but was Grade 3 and had a cough with mild sputum for a day. He came back to Gwalior his hometown by 10th evening. He was on Amoxiclav, Deriphylline and Terbutaline. His shortness of breath gradually reduced (Grade 2) and SpO2 was 98% by 13th August. Here his WBC count was 21,000/cumm, 4.42 lakhs platelets, Hb 14 gm% and his first X-ray chest was done. (Figure 1)

On 15th he noticed swelling of his right leg and went to a local hospital for further check-up. In the meantime, his swelling extended to his entire right lower limb. It was a non-pitting type except around the ankle. Colour Doppler of his right lower limb was done on 18th which showed evidence of profoundly hypoechoic thrombus in right external iliac veins distending the veins with no observable flow in them. Right common femoral, superficial femoral, deep femoral vein were also completely thrombosed with loss of compressibility and he was started on Injection. Meropenem 500mg I.V T.I.D, Tablet. Dabigatran 110 mg B.I.D, and Enoxaparin (40mg 8 injections S.C). On 22nd August patient, he got bouts of bleeding in stools. 3 episodes in a single day with massive blood loss causing his Hb to fall from 12 to 5.5 gm%. It was frank red in colour. Dabigatran and Enoxaparin were stopped, and he was put on Piperacillin and Tazobactam. 2 units of Packed Red Blood Cells were transfused on 24th and 25th August. And, his swelling reduced by 25th August and was present only around the ankle and foot. He still had a fever and grade 2 shortness of breath. He was advised to shift to higher centre and so the patient went to Delhi. (Figure 2 and 3)
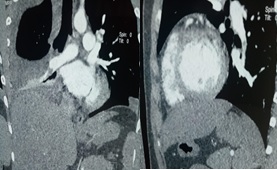
Upon admission, one more unit of PRBC was transfused. His ECG showed Sinus Tachycardia, S1Q3T3 pattern and a CT-Pulmonary Angiography was done and
Figure 2: Chest X-ray PA view taken on 24th August showing right sided pleural effusion.

Figure 3: ECG Done on 24th August showing Sinus Tachycardia and S1Q3T3 pattern.

Figure 4: CT-Pulmonary Angiography Images taken on 26th August showing a linear filling defect in right descending pulmonary artery suggestive of thrombus.
On 14th September (Figure 5) patient was admitted in our hospital and had complaints of low-grade fever, grade 2 Shortness of breath and right lower limb swelling. His Hb was 10.6gm%, TLC was 10800/cu mm, and platelets count was 6.5 lakhs/cumm. He was on Tablet. Dabigatran 110mg BID, Tablet. Clopidogrel 75mg, Tablet. Aspirin 150mg OD. In view of pleural effusion, a USG guided pleural tap was attempted, but no sample could be drawn due to loculations. Sputum for AFB was sent, as Pulmonary Tuberculosis was suspected but it was negative. Patient was discharged with Tablet. Warfarin 5mg OD instead of Tablet. Dabigatran 110mg for cost-
Figure 5: Chest X-ray PA view taken on 14th September showing right sided pleural effusion.
 efficacy. Presently patient is relieved of his
symptoms of fever, breathlessness and
lower limb swelling. His chest x-ray on 10th
November (Figure 6) showed complete
resolution of pleural effusion. His platelet
counts came back to normal range soon
after. As his platelets came back to normal
within 3 months, the diagnosis was
labelled as Reactive thrombocytosis due
to PE.
efficacy. Presently patient is relieved of his
symptoms of fever, breathlessness and
lower limb swelling. His chest x-ray on 10th
November (Figure 6) showed complete
resolution of pleural effusion. His platelet
counts came back to normal range soon
after. As his platelets came back to normal
within 3 months, the diagnosis was
labelled as Reactive thrombocytosis due
to PE.
Discussion:
The diagnosis for this patient was labelled as high-altitude pulmonary oedema (HAPE) with Thromboembolic disorder and Reactive Thrombocytosis. HAPE is a common condition which occurs in people who ascend to high altitudes at a rapid rate and are not acclimatised. Pulmonary Embolism (PE) has been uncommonly reported in few of these patients.
Figure 6: Chest X-ray PA view taken on 10TH November 2018 showing complete resolution.




Considering the lack of clear association between altitude and PE and the prevalence of HAPE as a cause of respiratory distress from altitude, there is often great difficulty in deciding which patients to evaluate for PE in this setting.6 In the present case, it could not be confirmed whether the patient had HAPE at presentation. Initially on descent, his breathlessness did not subside completely and as he developed fever and raised leucocyte count, he was suspected to have pneumonia and was treated with empirical antibiotics. But further his symptoms did not improve and in view of Deep vein thrombosis (which was confirmed by Colour Doppler), ECG changes of sinus tachycardia and S1Q3T3 pattern, patient was taken up for CT-PA which showed a thrombus in his pulmonary artery. All his symptoms, that is fever, cough, breathlessness and lower limb swelling could be attributed to his thromboembolic disorder, which he developed probably due to his visit to high altitude. A case series of 303 patients with HAPE showed that 8 patients had PE and
the cause was multifactorial.6 Travel to altitude increases PE risk, there are aspects of altitude excursions that increase blood viscosity, for example, dehydration causing haemoconcentration, and polycythaemia, in addition to the compensatory rise in haematocrit with acclimatization, which are likely to increase PE risk. One possible risk factor in this patient is prolonged travel on a motor bike during his visit to Ladakh and other areas. We must suspect PE in patients presenting with symptoms suggestive of HAPE who do not improve or get worse with descent within 24 hours and if possible, try to confirm the diagnosis. The patient had bouts of mucosal bleeding from his rectum probably due to the combination of Dabigatran and Enoxaparin. There is an additive effect of Dabigatran anticoagulant activity and residual anticoagulant activity from Enoxaparin.7 In view of this , it may be better to give Enoxaparin for 2 days followed by Dabigatran. In our patient we started Warfarin and stopped Dabigatran as studies show that Dabigatran even though it is not inferior to warfarin, has increased risk of acute coronary syndrome8 , and is at the same time much costlier than Warfarin.
In view of the significant mortality and morbidity associated with Pulmonary Embolism, it is advisable to have a high index of suspicion for PE in any patient of suspected HAPE whose symptom of breathlessness does not subside on descent, especially in patients with risk factors for hyper-coagulopathy.
Author Contributions:
Conceptualization: L.S.R., M.M.R,; Writing Original Draft Preparation: L.S.R., A.S.G., Data Acquisition and Analysis: A.S., M.M.R., L.S.R.; Writing-Review & Editing: A.S., A.S.G.; Images: A.S.G., A.S., M.M.R.
References
- Paralikar, S. (2012). High altitude pulmonary edema-clinical features, pathophysiology, prevention and treatment. Indian Journal of Occupational and Environmental Medicine, 16(2), p.59.
- Maggiorini M, Bühler B, Walter M, Oelz O BMJ. 1990 Oct 13; 301(6756):853-5.
- Hackett PH, Rennie D Am J Med. 1979 Aug; 67(2):214-8.
- Singh I, Roy SB. High altitude pulmonary edema: Clinical, hemodynamic, and pathologic studies. In: Command UA, Ra D, editors. Biomedicine of high terrestrial elevation problems. Washington D.C: 1969. pp. 108–20
- Dickinson J, Heath D, Gosney J, Williams D Thorax. 1983 Sep; 38(9):646- 56.
- Pandey, P., Lohani, B. and Murphy, H. (2016). Pulmonary Embolism Masquerading as High Altitude Pulmonary Edema at High Altitude. High Altitude Medicine & Biology, 17(4), pp.353-358.
- Clemens, A., van Ryn, J., Sennewald, R., Yamamura, N., Stangier, J., Feuring, M. and Härtter, S. (2012). Switching from enoxaparin to dabigatran etexilate: pharmacokinetics, pharmacodynamics, and safety profile. European Journal of Clinical Pharmacology, 68(5), pp.607-616.
- Ogbonna K, Dixon D. Critical appraisal of dabigatran in the treatment of deep vein thrombosis and pulmonary embolism. Journal of Blood Medicine. 2015;:177


