CASE RECORD
Case Records of Kamineni Institute of Medical Sciences Narketpally: A Woman with Progressive Abdominal Pain
*Gousia Ummae Salma Shaik1
*1Post graduate, Department of General Medicine, Kamineni Institute of Medical Sciences, Narketpally
*Corresponding Author
Gousia Ummae Salma Shaik
Department of Internal Medicine,
Kamineni Institute of Medical
Sciences, Narketpally, India - 508284.
Email: drshaiksalma@gmail.com
Abstract
The learning ecosystem of any medical college depends on how the students and faculty learn from their regular clinical individual patient based problem solving workflow. The study of actual cases of various diseases has been an effective way of making small steps towards a better medical teaching and a learning system. When such actual cases are presented as case records it brings out together the experience of various practitioners involved with the patient, and the discussions illustrate their decision- making process, their understanding of the literature around the disease affecting the patient, the further approach and management of the disease. This experience and knowledge could be applied to treat different cases which are involved with multiple factors of not a single disease entity but various diseases.
We describe the case record of a 40-year-old female from West Bengal who had presented with severe abdominal pain for the past 2 months. A set of radiological investigations were carried out which included an Ultrasound abdomen revealing findings suggestive of right ovarian tumor, which was later followed by an MRI which had revealed a long vascular pedicle to an enlarged right ovary. In view of her severe abdominal pain, a clinical diagnosis of ovarian torsion was suspected which was followed by the decision to do an emergency exploratory laparotomy, The ovary sample was sent for a histopathological investigation.
Key words:Case record, abdominal pain, fibrothecoma, lymphadenopathy, laparotomy, ovarian torsion, pain management, cancer pain.
Introduction
The learning ecosystem of any medical college depends on how the students and faculty learn from their regular individual patient based problem solving workflow. One way of sharing that learning experience is to document and share it on a journal platform for wider discussion, understanding and feedback. While this journal is not the first one to start this learning feature and there have been other illustrious and impactful examples before it.1,2 We hope to scale this feature in a manner that can directly impact our current local learning ecosystem and help us progress towards a better knowledge gaining experience.
Formal Structured Case Narrative:
This was a 40-year-old female who had travelled from West Bengal to our hospital as she had been suffering from pain in the right hypochondrium and pelvis radiating to the back since the past 2 months. She also had complaints of pain in the left hypochondrium and loin since the past 15 days. The pain was of continuous in nature, spasmodic type, with no aggravating or relieving factors noted. She had also complained of fever which was low grade especially in the evenings, associated with chills and rigors since the past 2-3 months. She gave history of weight loss in the past few months associated with decreased appetite and disturbed sleep. She attributed the disturbed sleep to the increasing intensity of pain in the abdomen. For the immediate symptomatic relief of pain she was given a Buscopan injection.
Later she underwent an ultrasonogram (USG) of the abdomen which revealed an endometrial polyp and a intramural fibroid with fluid in the pouch of Douglas and right-sided loculated pelvic fluid collection. The ultrasonogram also revealed findings of an enlarged right ovary with central hypervascularity, which was suggestive of a possible ovarian neoplasm. On the same day, a MRI of the pelvis was done revealing an enlarged right ovary and a heterogeneous lesion of 46x35mm with solid component and small cystic areas. (Figure 1) A long vascular pedicle to the right ovary was also noticed. It also confirmed the presence of a loculated collection in the pelvis. In view of her severe abdominal pain that was initially suspected to be an ovarian torsion, she was immediately operated. Exploratory laparotomy with right salpingo oophorectomy and left ovarian drilling was done. (Figure 2, 3, 4). The resected right ovarian mass was sent for a histopathological investigation. (Figure 5).
Postoperatively, she had developed fever, hypotension, and tachypnea. For the postoperative abdominal pain management, she was started on Tramadol injection 8th hourly and our Internal medicine department was requested to visit her and evaluate for the abnormal breath sounds and hypotension. The case was then taken up by our department for further management. We had advised to resuscitate her with fluids and to monitor her Blood Pressure regularly. A chest x- ray was advised as we could appreciate on auscultation and we had also sent her routine urine examination as we suspected in the Foley’s catheter.
Figure 1: showing enlarged right ovary with a heterogeneous lesion with solid component and a small cystic area

Figure 2, 3, and 4: showing intraoperative images during right salpingo oophorectomy and left ovarian drilling.

Figure 5: showing the resected right ovarian mass sent for histopathology.

She was shifted to our Intensive Care Unit as she had persistent hypotension despite of fluid resuscitation. We had started her on ionotropic support for her hypotension. We were successful to wean off her ionotropic support in 1 day, her blood pressure was maintaining around 120-130 mm Hg of systolic pressure in both the arms and 90 mm Hg of diastolic pressure. She still had persistent abdominal pain and pleuritic- chest pain, for which a combination of Tramadol and Paracetamol was added every 6 hourly and a Fentanyl patch was applied. Subjectively the patient had decreased intensity of pain, and clinically she had decreased intensity of sounds in bilateral infraaxillary areas with crepitation heard bilaterally in the mammary areas. The chest radiograph showed patchy infiltrates (figure 6) which warranted a Pulmonologist’s opinion.
Figure 6: showing patchy infiltrates in both lungs.

The Pulmonologist had found a few significant enlarged cervical lymph nodes which were missed during our initial evaluation and she was advised for sputum for acid-fast bacilli (AFB), Pleural fluid aspiration and a fine-needle aspiration (FNAC) of the enlarged cervical lymph nodes. An ultrasound chest was also advised which revealed bilateral minimal pleural effusion. We had two differentials for her patchy chest infiltrates in the background of her enlarged cervical lymph nodes and severe abdominal pain. The first being disseminated tuberculosis (TB), and the second being a secondary metastasis from the ovary. But in the view of her severe abdominal pain radiating to the back inspite of adequate coverage of analgesics, the probability of ovarian malignancy was high. Yet we were far from the diagnosis of the ovary specimen which had been sent for a biopsy after the emergency laparotomy.
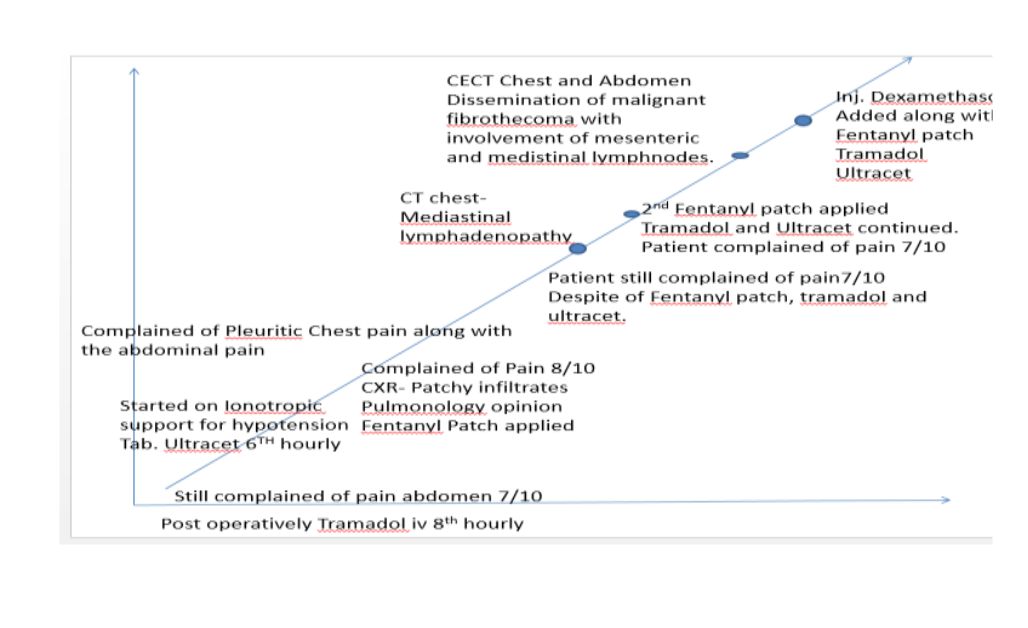
The patient continued to have fever spikes despite being on IV antibiotics although her sepsis and hypotension had reduced. She still was complaining of persistent pain despite being on adequate analgesia with a Fentanyl patch, oral Tramadol and Paracetamol combination (figure 7, 8). We had decided to reapply a second Fentanyl patch which was difficult to procure in our hospital.
Figure 7 and 8: showing the patient continued to have fever spikes

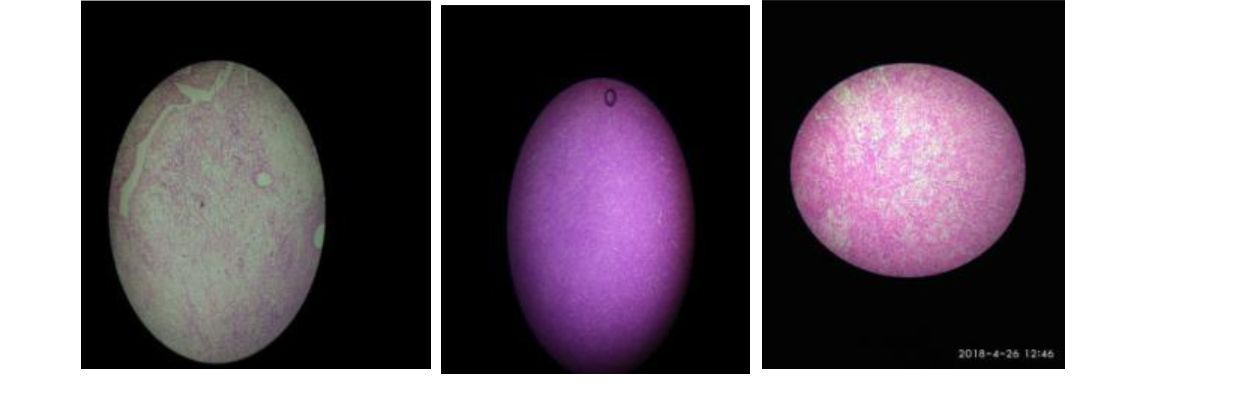
There was now an interesting turns to the case as we got the microscopic pictures (figure 9, 10, 11) of the right ovary, which we had attained on our visit to the pathology department for the histopathological opinion. The microscopic images had confirmed the diagnosis of Malignant Fibrothecoma.
Figure 9, 10 and 11: showing histologic findings of the right ovarian mass
In the meanwhile, we had got a contrast enhanced computed tomography (CECT) of her chest to note the dissemination of the malignancy if present, as we were wiser now with the histopathological diagnosis of the Malignant Fibrothecoma. The CECT of the chest showed bilateral pleural effusion and mediastinal lymphadenopathy (figure 12), suggesting a metastasis of the malignancy into mediastinal lymph nodes.
Figure 12: CECT of the chest is showing pleural effusion and mediastinal lymphadenopathy.s

How do we make sense of her fibrothecoma of the ovary, pulmonary nodules and pleural effusion and her severe abdominal pain? An MBBS short note often asked in the OBG exams by the name of Meigs syndrome suddenly rang a bell. In search of similar patient reported elsewhere, we found a case report presented with a thecoma and abdominal pain due to sclerosing peritonitis, similarly, to our patient. 3,4
By the time, we got the diagnosis of malignant fibrothecoma, we searched for any similar case reports describing dissemination of this malignancy to lymph nodes and found a similar article of a 50- year-old postmenopausal lady with a luteinizing thecoma and sclerosing peritonitis. (Figure 13, 14).5 Our patient had lymph node involvement and probably even the sclerosing peritonitis which aptly explains her abdominal pain.
Figure 13 and 14: showing a similar case report being presented

Informal Empathic Narrative: It was embarrassing to have the delayed realization of having missed such a glaring finding of lymphadenopathy in her neck during the admission day as we were overly distracted by her severe abdominal pain mimicking ovarian torsion. Our surgery residents had rectified it by obtaining an FNAC of the enlarged lymph nodes and painstakingly attempted to take lymph node excision biopsy and the macroscopic appearance of the sample is shown here (figure 15).
Figure 15: showing macroscopic appearance of the excision biopsy sample of right cervical lymph node.

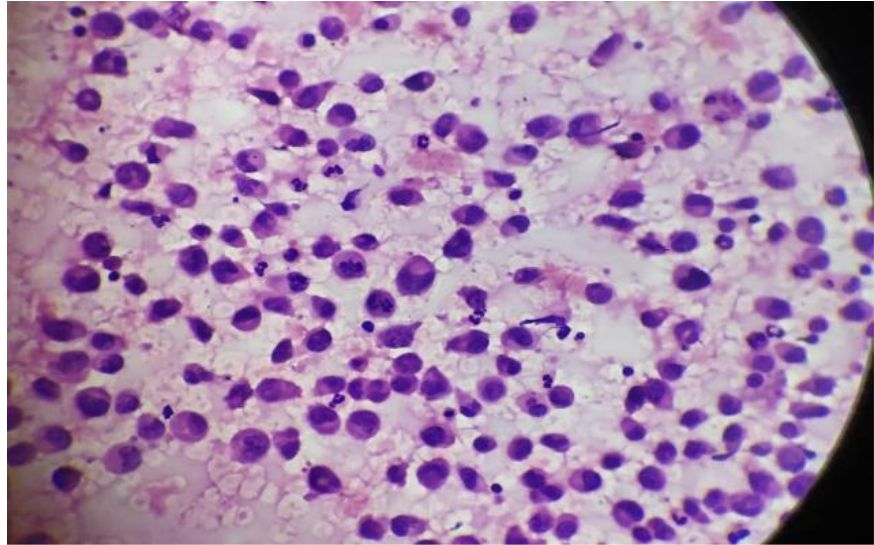
However, unfortunately we were appalled to learn from pathology department that the entire sample of the lymph node was spoilt and was unreportable as it had not been preserved in formalin. We all had the FNAC of right cervical lymph node as shown here (figure 16). The findings were inconclusive if this was a secondary metastasis from the same ovarian fibrothecoma pathology described earlier.
Figure 16: showing the FNAC findings of the right cervical lymph node.
The other close differential for our patient that came into consideration was Castleman disease, which has diverse manifestations with the ability to affect any body region, mimicking of both benign and malignant findings in the neck, chest, abdomen, and pelvis. “Castleman disease includes a spectrum of pathologic variants, including the classic hyaline vascular Castleman disease and the less common plasma cell Castleman disease.”6 Here too ours appears to fit into the less common variety of this uncommon disease. We were trying to relieve her of the pain which she continued to have despite all the possible analgesic treatment.
On a night duty day in ICU after explaining the nursing staff about the investigations to be sent the coming morning for the patients in the ICU, and the necessary work to be completed before the dawn arrives, I had left to my duty room to catch a nap as I had a long day coming ahead. It was almost 1 hour later when I got a call from the ICU asking me to attend a patient as her blood pressure and pulse were not recordable. Still in half sleep struggling to open my eyes and getting my senses into place I tried to recall what would have happened to her as I had seen her 1 hour back wincing out loud in pain. I rushed to the ICU where I see 2 persons from the nursing staff trying to wake her up, shouting out loud, while the other nursing person had understood the scenario and had arranged the CPR and the intubation tray with the necessary equipment.
I could sense the shiver in my spine and my heart shouting out loud, "Is this the end?" While I was going ahead with the CPR with the nursing persons in turns. Had called my team members to ICU urgently who were on duty that particular gloomy night. My team had arrived half exhausted half asleep after a long day, they assisted us in the CPR where all of us took turns in reviving her. I could see the questions in every one's eyes probably asking each other with their eyes whether is this we had imagined. After trying to revive her for 40 min we had taken the call to declare her dead. The nursing staff had handed over me a bunch of papers to be filled, the formalities to be completed, the calls to be made to intimate the administration about the death, the search for the closed ones of the deceased.
While I was filling the papers and completing the formalities I asked the staff there to call up the administrator on duty as I knew we would know what exactly had to be done after the formalities. The closed ones rushed in with so much fear in their eyes as they had been woken up from their sleep stating the urgent need of them in the ICU. Still completing the papers I see the son who rushed to his mother and shaking her up vigorously shouting out to wake her up, with tears rolling down his eyes he still was trying to wake her up, his wife had left to intimate their relatives 2000 kms away from this hospital about the unfortunate dawn which they had expected to occur but probably some months later.
My eyes filled up with tears on seeing a son a loved one trying to wake his mother up from a deep sleep from which no one has come back. He had booked his tickets to go to their home town with the patient along 4 days later. Nevertheless he hadn't wondered in his frightest thought about the end being so near. I sat there with a sad heart recalling the previous night when I had seen her and imagined in the fraction of minute as to how painful it was for her, she couldn't sleep nor could she sit. She couldn't breathe but nor did she want an oxygen mask over her face. We had inserted a Ryle’s tube suspecting an intestinal obstruction and she begged us to remove it that night. She had begged her son to remove it but he didn't want to do so and neither could he explain his mother that removing it was not a wise decision. All these ran through my mind when I hear my phone ring. I got a call from Casualty asking for help for a case.
On my way to casualty I once again got reminded of how imprecise medicine was. We had a lady suffering with a disease in the end stage and all we had to do was to make her last days comfortable, which we were unsuccessful at. Because in the recent few days we had done a biopsy of her lymph node, loaded her with intravenous contrast for the radiology imaging, tried securing cannulas so many times in her edematous limbs. She had definitely gone through much pain in the last few days. The imprecision of the medicine again stands up, as we knew what she was suffering from, but could we help her? Could we provide the peace and comfort in her last few days on this Earth? Could we assure her with precision that you will be living for these many months or years.., we could do nothing? Nothing which would have helped her or which would have comfort her.
Patient-Centered Discussion:
Flashing back to her deadly cancer causing a severe pain, we wish we could do better and thus, sharing our understanding of how we may approach similar patients with terminal cancer pain. Management of cancer pain is multifaceted requiring more than just an analgesia ranging from antineoplastics (treating the malignancy itself), pharmacotherapy (analgesics and other adjuvants), interventional and psycho- behavioral management to hospice care. In the pain management, assessment of the severity of pain is important for which are available different scales like visual analogue scale, verbal scale and numerical scale. [Figure 17] How do we approach to patient after an assessment of the pain? We may require just analgesics or may even non-pharmacological modalities like various injections, neuroablative and neurostimulator techniques and psychological interventions. What could actually be End of life pain in a patient who probably is at the end? “53%–70% of patients with cancer- related pain require an alternative route for opioid administration in the months and hours before death. Pain is often accompanied by other symptoms such as dyspnea, agitation, and anxiety, any of which can exacerbate underlying central pain mechanisms.”7 In our patient as we recall had all of the above. In this situation, sedation may be the only therapeutic option capable of providing adequate relief. The justification of sedation, which should bear are intervention for pain, is that it is an appropriate and proportionate goal.
Figure 17: showing different scales of assessing pain severity.

According to WHO ladder for analgesia,8 the cancer pain can be managed categorizing the pain by its severity. For mild pain, which is quite unlikely in cancer patients though, one could start initially with paracetamol and NSAIDs or their combination. For mild-moderate pain, the choice of analgesic drugs could range from tramadol, dihydrocodeine and codeine. For severe pain, strong opioids are the option. A Cochrane systematic review published in 2016 analyzed 62 studies with 4241 participants and supported the use of oral morphine as an effective analgesic for cancer pain, with a low rate (6%) of reported intolerable adverse events. Transdermal fentanyl also achieved similar rates of effective analgesia and has also been advocated as an effective and tolerable analgesic. [8] With the various complexities of patients and individual variation of the cancer pain, choice of opioid requires an optimal balance between analgesia and unwanted adverse effects.
What is BTcP? BTcP is Breakthrough cancer pain. There is no unanimous consensus on definition and characteristics of BTcP. But BTcP defined as an episode of severe pain that occurs in patients receiving a stable opioid regimen for persistent pain sufficient to provide at least mild sustained analgesia.7 Now after this interpretation of BTcP could we tell that our patient was suffering from this? Well probably yes, now how could we have gone ahead in such a scenario? Several placebo-controlled RCTs have demonstrated the efficacy of all available transmucosal fentanyl formulations for BTcP. But these products have been tested only in opioid-tolerant patients, the current recommendation is only for patients receiving doses of oral morphine equivalents of at least 60mg. But we didn't have access to such transmucosal and intranasal fentanyl patches so we had only managed with the transdermal fentanyl patch. The entire course of events in terms of management has been reflected in this graph here [figure 18]
Figure 18: showing graphical presentation of the course of events occurred in this patient.
Conclusion
Medicine has advanced so ahead in the past few years but still we could do nothing to help her, to soothe her pain. She had come all the way from her home town travelling for 2 days to help get rid of her pain which she had been having since the 2 months. Has medicine given her the intimation of the precise time which she was left with? Probably this is the way it works, being imprecise, striving for precision, because medicine cannot intimate a person regarding the precise time one has been left with. Would precision in such events of life and death help us in any way or is it better to be imprecise in few areas of life is left for us to decide. Despite all the efforts we could not soothe her pain and save her life. The imprecision of the medicine again stand up, as we knew what she was suffering from, but could we help her? Could we make the end-of-life care better for her? Could we assure her with a precision that for this specific time period she will be living? A new dawn for everyone but sadly for a family it had been quite unfortunate.
References
- Harris NL. Case records of the Massachusetts General Hospital— continuing to learn from the patient. N Engl J Med. 2003; 2252-2254
- Case Records of the Massachusetts General Hospital (Case 17-2003). N Engl J Med 2003;348:2239-2247
- Bahar B, Hu Z, Szpaderska A, Liotta M, Potkul RK, Smith D, Ersahin Ç. Fatal case of luteinized thecoma with sclerosing peritonitis in a 40-year-old woman. International Journal of Gynecological Pathology. 2014 Jan 1;33(1):30-4.
- Fernández-Alba JJ, Vilar A, González- Macías C, Hens A et al. Fatal Case of Bilateral Luteinized Thecoma with Sclerosing Peritonitis in a 33-Year-Old Woman. Austin J Obstet Gynecol. 2015;2(1): 1034.
- De A, Mukhopadhyay S, Nandi A, Das I. Sclerosing peritonitis with unilateral ovarian luteinized thecoma in a post- menopausal woman: A case report. Journal of mid-life health. 2014 Oct;5(4):198.
- Bonekamp D, Horton KM, Hruban RH, Fishman EK. Castleman disease: the great mimic. Radiographics. 2011 Oct 4;31(6):1793-807.
- Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti CI, ESMO Guidelines Committee. Management of cancer pain in adult patients: ESMO Clinical Practice Guidelines. Annals of Oncology. 2018 Jul 24;29(Supplement_4):iv166-91.
- Wiffen PJ, Wee B, Derry S, Bell RF, Moore RA. Opioids for cancer pain–an overview of Cochrane reviews. Cochrane Database Syst Rev. 2017 Jan 1;7.


