Case Report
APLA NEGATIVE APLAS
Kodi. Vinuthna,1, Madhumitha choudhary2, Madhava Sai Sivapuram3
1Post Graduate, Department of General Medicine, Kamineni Institute of Medical Sciences, Narketpally, Telangana
2 Department of General Medicine, IQ City Medical College, Durgapur, West Bengal.
3* Department of General Medicine, Dr. Pinnamaneni Siddhartha Institute of Medical Sciences and Research Foundation, Chinna-Avutapalli, Andhra Pradesh.
*Corresponding Author
Madhava Sai Sivapuram *
Department of General Medicine,
Dr Pinnamaneni Siddhartha Institute of Medical
Sciences and Research Foundation,
Chinna-Avutapalli,
Andhra Pradesh, India-521101
Email: madhavasai2011@gmail.com
Abstract:
Background: Antiphospholipid antibody syndrome (APLAS) is a clinical condition characterized by recurrent vascular thrombosis along with pregnancy-related complications with raised antibodies against phospholipids. Very rarely we come across a clinical profile of APLAS but not satisfying the diagnostic criteria, such cases are termed as seronegative APLAS. Case presentation: A 28 Years old female presented to the emergency with altered sensorium and slurring of speech for one week. The patient has a significant history of two abortions and a pre-term delivery. Following that she developed acute kidney injury which progressed to chronic kidney disease (CKD). For CKD patient is still on dialysis. Diagnostic workup showed negative antibodies for the phospholipids. Due to the clinical significant history and symptoms with negative diagnostic workup, it was diagnosed as seronegative APLAS.
Introduction:
The history of antiphospholipid antibody syndrome (APLAS) started around 20 years back. (1) APLAS is an autoimmune disorder characterized by recurrent vascular thrombosis along with pregnancy comorbidities like recurrent abortion before 10weeks, abruptio placenta secondary to pregnancy-induced hypertension, preterm delivery, and IUGR. (2) Raised antibodies against phospholipids are required for diagnosing APLAS. But in clinical practice, there has been a discrepancy between the detection of antibodies and disease presentation which gave rise to a new group of seronegative APLAS or APLA negative APLAS. (3) Seronegative APLAS was first introduced by Huges and Khamashta in 2003. (1) Patients having clinical symptoms suggesting APLAS but on testing for antibodies turned negative are The history of antiphospholipid antibody syndrome (APLAS) started around 20 years back. (1) APLAS is an autoimmune disorder characterized by recurrent vascular thrombosis along with pregnancy comorbidities like recurrent abortion before 10weeks, abruptio placenta secondary to pregnancy-induced hypertension, preterm delivery, and IUGR. (2) Raised antibodies against phospholipids are required for diagnosing APLAS. But in clinical practice, there has been a discrepancy between the detection of antibodies and disease presentation which gave rise to a new group of seronegative APLAS or APLA negative APLAS. (3) Seronegative APLAS was first introduced by Huges and Khamashta in 2003. (1) Patients having clinical symptoms suggesting APLAS but on testing for antibodies turned negative are grouped under this Seronegative APLAS. (3) To increase the awareness of the seronegative APLAS the authors presented this case of 28 years old female with arterial and venous thrombosis and pregnancy-related complications with negative antiphospholipid antibodies.
Case report:
A 28 Years old female G3P1L1A2 presented to the Emergency ward in May of 2017 with altered sensorium since one day and slurring of speech from the last one week. Upon further inquiry, the patient’s family provided us with a significant history of two abortions, six months apart during the year 2014-15. She conceived for the third time in August of 2015. She developed hypertension during her fourth month of gestation. She was taken for emergency LSCS at 33 weeks of gestation due to abruption of the placenta in April of 2016. Postpartum day one, the patient developed generalized edema, oliguria, was diagnosed as Acute Kidney Injury (AKI) and taken for dialysis. AKI progressed to Chronic Kidney Disease (CKD) due to the renal artery thrombosis (RAT) and the patient is on maintenance dialysis till today. Four months later in August of 2016, she developed right thigh pain, diagnosed as DVT of right femoral vein for which she took anticoagulants for three months and stopped later. In February of 2017 patient developed sudden painful loss of vision in her left eye diagnosed, as pan-uveitis progressed to endophthalmitis and enucleation was done. Her histopathology report of the eye showed end-stage eye disease with degeneration. Three months later in May of 2017, she developed speech disturbance, which was sudden onset, non-fluent and interrupted by pauses. On examination, she was drowsy, not oriented to time, place & person. She was pale and icteric with bilateral pedal edema. Higher mental functions, cranial nerves, the sensory system could not be assessed as the patient was disoriented and motor system tone was normal with normal reflexes. Fundoscopy of the right eye was normal.
Investigations:
During May of 2017, the following laboratory investigations revealed hemoglobin 7gm% and platelets 78,000/μl. Her ESR was 110mm in 1st hour and peripheral smear showed schistocytes. Reticulocyte count was 4% with coombs test being positive. Her LDH was elevated with 3,720 IU/L. Her renal parameters were deranged with blood urea 70mg/dl and serum creatinine 6.2mg/dl. Her serum bilirubin was elevated 7.2 mg/dl with indirect bilirubin 6.1 mg/dl. Her prothrombin time was 14.6 sec (reference 9.5- 12.2 sec) and International Normalized Ratio (INR) was 1.16. Her Renal Function Tests showed blood urea of 70 mg/dl and serum creatinine 6.2mg/dl. CT brain showed no hemorrhage and MRI brain showed acute infarcts in the right parietal and temporal lobes. Her serum ANA was negative, IgG for anticardiolipin was negative, lupus anticoagulant was negative and IgG beta 2 glycoprotein was negative.

Figure 1: CT brain showed no hemorrhage
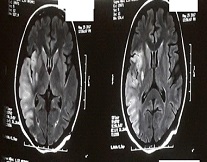
Figure 2: MRI brain on presentation showed acute infarct in right parietal & temporal lobes
Treatment:
Patient continued on dialysis for renal failure. Speech therapy along with antiplatelets was started. Aspirin 75 mg/ day along with unfractionated heparin was given for 5 days, bridged to warfarin 4mg OD and INR was maintained between 2-3.
Discussion:
APLAS is also known as Hughes syndrome diagnosed based on the Sapporo criteria. Sapporo criteria consist of clinical findings such as vascular thrombosis and recurrent pregnancy-related complications and the following laboratory findings: the presence of lupus anticoagulant, anticardiolipin antibody, or anti-β2 glycoprotein 1 antibody. (4) Sometimes, physicians come across patients where they strongly suspect of having APLAS but who do not satisfy the laboratory criteria. For such suspected cases, a subtype of APLAS termed seronegative APLAS has been proposed by Hughes. In our patient, the problem started from 2014 with a significant clinical history presenting with 2 abortions, preterm delivery due to abruption of placenta, renal failure, deep vein thrombosis, cerebrovascular accident (CVA) secondary to the middle cerebral artery, uveitis leading to endophthalmitis. Our patient clinically fits into APLAS, but laboratory evidence came out to be negative. This is due to the involvement of several other antigens besides those mentioned in the Sapporo criteria. Antibodies may be directed against other phospholipids like phosphatidylethanolamine, or against components of the protein C pathway or annexin V.(5) Although these molecules can increase the diagnostic yield of APLAS, their clinical relevance is still debatable and needs to be confirmed. (6) So with this case report, we would like to acknowledge that seronegative APLAS is a clinical condition that can occur with the positive clinical finding of APLAS with negative diagnostics and patient should be treated accordingly to prevent further complications.
Conclusion:
A 28-year female G3P1L1A2 presented to the emergency ward with a significant history of altered sensorium and slurring of speech. She also has a significant history of abortions, pre-term delivery following that on AKI and slowly progressed to CKD due to RAT. Following that she has developed uveitis and enucleation was done. Based on clinical findings patients were suspected to be APLAS clinically. Upon further investigating for antibodies to confirm, her serum ANA was negative, IgG for anticardiolipin was negative, lupus anticoagulant was negative and IgG beta 2 glycoprotein was negative. Due to the clinically significant symptoms, the patient was diagnosed as seronegative APLAS and further appropriate treatment was provided to prevent further complications.
References
- Hughes GR V, Khamashta MA. Seronegative antiphospholipid syndrome. Ann Rheum Dis [Internet]. 2003 Dec [cited 2019 Aug 13];62(12):1127. Available from: http://www.ncbi.nlm.nih.gov/pubmed/14644846
- Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost. 2006 Feb;4(2):295–306.
- Nayfe R, Uthman I, Aoun J, Saad Aldin E,
Merashli M, Khamashta MA. Seronegative
antiphospholipid syndrome. Rheumatology
[Internet]. 2013 Aug 1 [cited 2019 Aug
13];52(8):1358–67. Available from:
https://academic.oup.com/rheumatology/article -lookup/doi/10.1093/rheumatology/ket126 - Saponjski J, Stojanovich L, Djokovic A, Petkovic M, Mrda D. Systemic vascular diseases in the antiphospholipid syndrome. What is the best diagnostic choice? Autoimmun Rev [Internet]. 2011 Feb [cited 2019 Aug 13];10(4):235–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21095242
- Conti F, Capozzi A, Truglia S, Lococo E, Longo A, Misasi R, et al. The mosaic of “seronegative” antiphospholipid syndrome. J Immunol Res. 2014;2014.
- Cervera R, Conti F, Doria A, Iaccarino L, Valesini G. Does seronegative antiphospholipid syndrome really exist? Vol. 11, Autoimmunity Reviews. 2012. p. 581–4.


