Current Issues
Case Report
Vulval cyst - A diagnostic dilemma
*Corresponding author
Dr Ramalingam P
Professor, Department of Surgery
Kamineni Institute of Medical Sciences, Narketpally, Nalgonda district,
Telangana state, India – 508 254.
Email: drram.pata@gmail.com
1Professor, 2Post Graduate, Department of General Surgery, 3Associate Professor, Department of Gynecology and Obstetrics, Kamineni Institute Of Medical Sciences, Narketpally, Nalgonda District, Telangana State, India.
ABSTRACT
Vulval cyst is very uncommon. Vulval cyst can be seen in many sites including face, trunk, and extremities but its occurrence in vulva is uncommon. This is the first case of epidermoid cyst of vulva reported in this region.
Key words : Bartholin’s cysts, lamellated keratin, post circumsicion cysts, pultaceous material, Vulva.
Introduction
Cystic masses of the vulva are relatively uncommon. Because of the rarity and diversity in etiology and pathology with simple presentation, it becomes a challenge and diagnostic dilemma to diagnose and treat appropriately. Here we are presenting, probably a first case report of epidermal vulval cyst.
Case Details
 A 60 year old female patient presented to the hospital with chief complaints of swelling in the pubic region since 18 years, with no other complaints. She had a marital life of 40 yrs with seven live children.
A 60 year old female patient presented to the hospital with chief complaints of swelling in the pubic region since 18 years, with no other complaints. She had a marital life of 40 yrs with seven live children.
Clinical examination showed a solitary oval swelling of size (9x7)cm extending from mons pubis on left side to the vulva lower down with no visible pulsations or peristalsis (Fig. 1). There were no signs of inflammation over the swelling and punctum was not seen.
On palpation it was found to be a soft cystic mobile swelling in the subcutaneous plane and skin was not fixed to the swelling.
Discussion
We present here a case of huge epidermal cyst measuring 9x7 cms probably the first in the literature. Various other cysts & swellings of various origins are reported in the literature. The differential diagnosis of vulval cysts include benign and malignant swellings like lipomas,1,3 liposarcomas,4-6 Bartholin’s cysts ± hydradenoma papilliform, mucinous vulvar cysts, inguinal hernias, obturator hernia,11,12 subpubic cartilaginous cysts,13,14 pseudosynovial cysts, subchondral cysts, Gartner’s cyst, Naboth’s cysts, Paratubal cysts, post circumsicional cysts 7-10 specially in Africa & epitheloid sarcoma which is more aggressive in genital region compared to other parts of body.
The frequently occuring Bartholin’s cysts usually occur in the lower half of the vulval region. Lipomas occur anywhere on the vulva, post circumcision cysts occur around the clitoris, whereas malignant & other skin conditions can occur anywhere.
Although careful physical examination is mandatory to avoid misdiagnosis, presentation of a swelling with soft consistency is sometimes difficult to differentiate clinically & need further investigations like USG, CT, MRI, Biopsy etc. Some conditions need simple excision and others need radical procedures.
Summary
 A 60 year old female patient presented to the hospital with chief complaints of swelling in the vaginal region since 18 years with no other complaints except that the swelling which was initially of 2x1cms had gradually progressed to present size of 9x7cms with no signs of inflammation. After preoperative consent and preparation, the swelling was explored and found to be a cyst with pultaceous material coming out of the opening (Fig. 2). This was excised completely with haemostasis.
A 60 year old female patient presented to the hospital with chief complaints of swelling in the vaginal region since 18 years with no other complaints except that the swelling which was initially of 2x1cms had gradually progressed to present size of 9x7cms with no signs of inflammation. After preoperative consent and preparation, the swelling was explored and found to be a cyst with pultaceous material coming out of the opening (Fig. 2). This was excised completely with haemostasis.
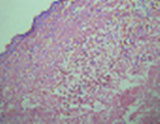
The excised specimen was sent for biopsy and histopathological examination revealed benign epidermoid vulval cyst (Fig. 3, 4). Post operative period was uneventful.
Though various conditions like lipomas,2 bartholin cyst, nabothion cysts, gartners cyst, mucinous cysts and hernias were reported in literature previously, there is no literature showing epidermoid vulval cyst and it may be the first case in this region.
 D
Differential diagnosis such as cystic neoplasm of pancreas, pseudo-cyst of pancreas, and pancreatic abscess were considered. USG guided FNAC was performed under strict aseptic conditions using an 18 gauge spinal needle. The aspirate revealed frank, thick pus, and the material was smeared on slides and stained with May-Grunwald-Giemsa (MGG) stain, and Ziehl-Neelsen (ZN) stain for acid fast bacilli (AFB). The smear showed degenerative / necrotic background loaded with acid fast bacilli on ZN stain (Fig. 2).
D
Differential diagnosis such as cystic neoplasm of pancreas, pseudo-cyst of pancreas, and pancreatic abscess were considered. USG guided FNAC was performed under strict aseptic conditions using an 18 gauge spinal needle. The aspirate revealed frank, thick pus, and the material was smeared on slides and stained with May-Grunwald-Giemsa (MGG) stain, and Ziehl-Neelsen (ZN) stain for acid fast bacilli (AFB). The smear showed degenerative / necrotic background loaded with acid fast bacilli on ZN stain (Fig. 2).
References:
- De Lima Filho OA, Cogliati AO, Reitzfeld G. Lipoma of the vulva. Rev Paul Med. 1969;75:165-76.
- Signorini M, Campiglio GL. Posttraumatic lipomas: where do they really come from? Plast Reconstr Surg. 1998;101:699-705.
- Copcu E. Sport-induced lipoma. Int J Sports Med 2004;25:182-5.
- Nucci MR, Fletcher CD. Liposarcoma (atypical lipomatous tumors) of the vulva: a clinicopathologic study of six cases. Int J Gynecol Pathol 1998;17:17-23.
- Rogers RG, Thorp JM., Jr Liposarcoma of the vulva: a case report. J Reprod Med.1995;40:863–864.
- Wu TC, Tarn JJ. Vulvar myxoid liposarcoma. Taiwan J Obstet Gynecol. 2007;46:293–294.
- Fox E F, de Ruiter A, Bingham JS. Female genital mutilation. Int J STD AIDS. 1997;8:599–601.
- Hanly M G, Ojeda V J. Epidermal inclusion cysts of the clitoris as a complication of female circumcision and pharonic infibulation. Cent Afr J Med.1995;41:22–24.
- World Health Organisation. A traditional practice that threatens health—female circumcision. WHO Chron. 1986;40:31–36.
- Egwuatu V, Agugua N E. Complications of female circumcision in Nigerian Igbos. Br J Obstet Gynaecol. 1981;88:1090–1093.
- Bjork K J, Mucha P Jr, Cahill D R. Obturator hernia. Surg Gynecol Obstet.1988;167:217–222.
- Jamadar D A, Jacobson J A, Morag Y, Girish G, Ebrahim F, Gest T. et al. Sonography of inguinal region hernias. AJR Am J Roentgenol. 2006;187:185–190.
- Alguacil-Garcia A, Littman CD. Subpubic cartilaginous cyst: report of two cases. Am J Surg Pathol 1996;20:975–979.
- Kier R. Nonovarian gynecologic cysts: MR imaging findings. AJR Am J Roentgenol.1992;158:1265–1269.


