Current Issues
Original Article
Perception of 1st year Mbbs students on Early Clinical Exposure with Horizontal Integration as a teaching Learning method
*Corresponding Author
Dr.N.Rajya Lakshmi,
Assistant Professor, Department of Biochemistry,
Kamineni Institute of Medical sciences, Narketpally, Nalgonda, Telangana state, 508 254, India.
Email Id: kota_kusum@yahoo.co.in
1Assistant professor, Dept of Biochemistry, 2Professor & HOD, Dept of Biochemistry, 3Professor of Biochemistry & Principal, 4Assistant professor, Dept of Anatomy, 5Assistant professor, Dept of Physiology, Kamineni Institute of Medical sciences (KIMS), Narketpally, Nalgonda, Telangana state, India.
Abstract
Back ground: Basic Science subjects are important in terms of giving a holistic approach to clinical problems. Need of the hour is to implement effective teaching learning methodologies which help students develop critical thinking skills. In the present study, evaluation of perceived effectiveness of Early Clinical Exposure (ECE) with horizontal integration of basic science subjects in 1st MBBS students was attempted.
Methodology: Two hundred 1st year MBBS students participated in present program. They visited hospital, presented cases and integrated seminars under the guidance of faculty. The perception of students towards the program was sought in form of 12-item questionnaire. Total of 185 students answered the questionnaire.
Results: Most of the students 84.3% (n=156) agreed that ECE with horizontal integration helped them to understand concepts better. Majority i.e. 93.5% (n=173) have expressed need to implement ECE and horizontal integration in curriculum. About 78.4% (n=145) agreed that the program motivated them to study basic sciences.
Conclusion: Introduction of ECE with horizontal integration of 1st MBBS subjects in the curriculum benefits the students in better understanding and provides a base for conceptual learning. These teaching learning methodologies complement the traditional didactic lectures in providing a successful integration of teaching and learning of basic sciences.
Key words: Basic sciences, Didactic lectures, Early clinical exposure, Horizontal integration, MBBS, Traditional questionnaire
Introduction
The authority model of teaching in medical colleges is teacher-centered and frequently entails lengthy lecture sessions or one-way presentations. Traditional teaching styles have evolved with the advent of differentiated instruction, prompting teachers to adjust their styles towards student’s learning needs.
For medical students to make competent clinical decisions based on sound scientific principles, they must be able to retain knowledge from the preclinical phase of their medical course1,2,3,4. Evidence from published literature indicates that failure rates in certifying examinations and board certification status were significantly associated with the assessment of retained basic sciences knowledge from medical school education.5
Teaching medicine especially basic science subjects in ways to make it interesting, enhance learning, conceptualize the knowledge and enable them to apply it in the medical field has always been a challenge. In order to meet the above challenges, there has been an increasing use of Early Clinical Exposure (ECE) and integrated teaching as educational strategies in recent years. Their use has also been recommended by the Medical Council of India (MCI) in the Vision 2015 document.6
Early Clinical Exposure (ECE) can be defined as a teaching-learning methodology, which fosters exposure of the medical students to the patients as early as the first year of medical college.6 In the traditional curriculum of medical education, MBBS students in their first year learn theoretical knowledge without contact with the patient in a clinical context. Moreover, in clinical fields they cannot recall important basic science concepts. Therefore, parts of their academic education become impractical.7, 8
The term integration in education means coordination in the teaching learning activities to ensure harmonious functioning of the educational processes.9 It is defined as organization of teaching matter to interrelate or unify subjects frequently taught in separate academic courses or departments.10 Integrated teaching aims to provide knowledge to the student which is in a complete, organized and wholesome manner, while the burden of integration has traditionally fallen primarily on the students.11 To put it simply, instead of imparting knowledge on a topic in a disintegrated manner, a particular topic can be taken by all the three departments of basic sciences (Anatomy, Physiology and Biochemistry) by forming a co-ordinated integrated teaching program. It is akin to different systems in our body working in a co-ordinated manner to achieve homeostasis.12 Medical Council of India in Vision 2015 suggests the incorporation of integration in the medical curriculum13, in order to provide the students with a holistic rather than a fragmented learning perspectives.14
Studies were done previously on individual ECE and integration, mostly vertical on the learning outcomes of MBBS student. Hence this study was designed to introduce ECE in combination with Horizontal integration of basic sciences in the 1st year of MBBS in our medical college in Nalgonda, India.
Aims and Objectives
To evaluate the perception of 1st year MBBS students on usefulness of ECE in improving the student’s learning process in basic sciences.
To evaluate the perception of the effectiveness regarding horizontal integration as an additive to ECE in improving their experience of the program.
To facilitate horizontal integration between disciplines and bridging the gap between theory and practical knowledge
Methodology
- Details of the activity: It is a coordinated activity by Preclinical, Para- clinical and Clinical faculties. An interdepartmental meeting was conducted for discussing the methodology, selection of topics and selection of core group members.
- Core group formation: This group included faculty from Anatomy, Physiology, Biochemistry and concerned Clinical subjects- Medical and Surgical disciplines.
- Grouping of the students: All the 200 students were divided into 5 groups with 40 students in each group; A (1-40), B(41-80), C(81-120), D(121-160), E(161-200). Each group was further subdivided into 4 subgroups with 10 students in each. Five (5) clinical topics which are to be included in the program were selected in the interdepartmental meeting and allotted to each group in the following manner (Table.1).
The 4 subgroups in each group were to prepare on different aspects of the allotted topic i.e. case presentation, anatomical aspect, physiological aspect and biochemical aspect.
Institutional ethical committee approval was taken. A total of 200 students participated in the program voluntarily.
table.1 clinical topics allotted to each group
| S.No. | topic | Group |
| 1 | Myocardial Infarction | A (1-40) |
| 2 | Diabetes Mellitus | B (41-80) |
| 3 | Jaundice | C (81-120) |
| 4 | Renal Failure | D (121-160) |
| 5 | Meningitis | E (161-200) |
Role of students
The students were assigned their topic and they were asked to interact with the faculty members of Anatomy, Physiology, Biochemistry and Clinical faculty based on the case for guidance in understanding, planning and presenting the topic in the large group. The group of students who belong to the clinical case category have to interact with the co-ordinator, who will guide them with the clinical case taking in the hospital and case presentation.
Role of co-ordinator and faculty members
Co-ordinator will co-ordinate with the faculty members, clinicians and students, thereby facilitating integration of the subjects and clinical case study. The faculty members facilitated the students in preparation and presentation of their respective topics with special emphasis on integrating the topic with other subjects and relating it with the clinical case.
Presentation
All the speakers got 15 mins to present their topic and were awarded participation certificate. The “Star performer” of the day was announced after the presentation and interaction session.
criteria for selection of “star Performer”
A panel of three Judges involving faculty as below:
- Judge No. 1: Faculty from Clinical Department
- Judge No. 2: Faculty from Para-clinical
- Judge No.3: Faculty from Preclinical Department
Each judge assessed all the speakers for 50 Marks (Total Marks 150) on the following guidelines.
- Subject Relevance
- Fluency and Diction
- Body Language
- Use of audio-visual aids
- Response to the queries
Department
10 students were randomly selected among the audience who voted and contributed in deciding the “STAR PERFORMER” of the day with 5 Marks per vote (50 Marks).
Total Marks: 200 Marks (150+50)
Evaluation of the program
After completion of all the topics the participants answered a validated questionnaire. A 12 item questionnaire which included structured questions was given to the students. Out of the 12 questions, 8 questions were framed in the form of a four-point Likert scale with a score of 1= Not at all, 2= Not to a significant extent, 3= To a significant extent and 4=To a great extent and 3 were polar questions (yes/ No). One question was framed for seeking an overall rating of the program on a Likert scale of 1=Poor, 2=Fair, 3=Good and 4=Excellent. The statistical analysis was done using percentage method.
Results
A total of 200 students of 1st MBBS (2015-2016) batch have participated in the program. The student’s perception of the effectiveness of the program was sought by a validated questionnaire. The completed questionnaires were returned by 185 students. A majority (90.2%, n=167) of the students gave an overall rating of the program as good to excellent on the four point Likert scale (1=poor, 4= excellent ) (Table.2)
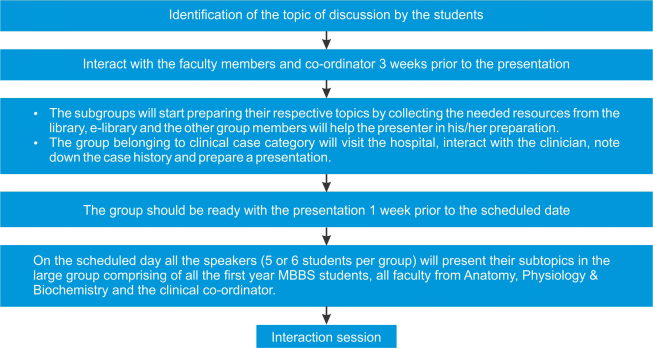
Fig. 1: Flow chart depicting the sequence of events in the program
The different aspects of the program which impressed the students and helped them in understanding the subject better were case based seminars, exposure to clinical subject, integrated approach and team work (Table.3).
table.2 Overall rating of the program by the students
|
Frequency | Percent |
| Poor | 6 | 3.2 |
| Fair | 12 | 6.5 |
| Good | 151 | 81.7 |
| Excellent | 16 | 8.6 |
| Total | 185 | 100.0 |
table.3.components of the program which impressed the students
| component | Frequency | Percent |
| Case based seminars | 25 | 13.5% |
| Exposure to the patients | 34 | 18.4% |
| Integrated approach | 26 | 14.1% |
| Team work | 31 | 16.8% |
| All the above | 69 | 37.3% |
| Total | 185 | 100% |
The distribution of various aspects of student’s perception towards early clinical exposure and integrated teaching are shown in Table 4. It shows students perception on factors such as better understanding of the subject, acquiring knowledge, development of interest in the subject, effect on their communication skills, development of sensitivity towards patient problems and needs, correlation of disease conditions with their theoretical knowledge, integration of the knowledge and change in their attitude towards importance of basic science subjects in medicine.
The different aspects of the program which impressed students and helped them in understanding the subject better were case based seminars (n=25, 13.5%), exposure to clinical subject (n=34,18.4%), integrated approach(n=26,14.1%) and team work(n=31, 16.8%). However 37.3% (n=69) of the students were impressed by all the above mentioned aspects of the program.
Majority of the students (84.3%, n=156) agreed that the program helped them in understanding concepts better when compared to the other topics where only traditional didactic teaching
table.4. students’ attitude towards the program (n=185)
| Variable | Not at all | Not to asignificant extent | To a significant extent | to a great extent | ||||
| No. | % | No. | % | No. | % | No. | % | |
| Understanding of the subject | 7 | 3.8 | 31 | 16.8 | 109 | 58.9 | 38 | 20.5 |
| Acquiring knowledge in the concerned topics | 6 | 3.25 | 41 | 22.2 | 115 | 62.2 | 23 | 12.4 |
| Developing interest in the subject | 20 | 10.8 | 48 | 25.9 | 81 | 43.8 | 36 | 19.5 |
| Developing communication skills | 35 | 18.9 | 36 | 19.5 | 61 | 33.0 | 53 | 28.6 |
| Developing sensitivity towards patient problems and needs |
33 | 17.8 | 38 | 20.5 | 60 | 32.4 | 54 | 29.2 |
| Motivated them to correlate the disease conditions with basic science subjects |
38 | 20.5 | 45 | 24.3 | 48 | 25.9 | 54 | 29.2 |
| Integrate the knowledge in the topics covered in ECE | 15 | 8.1 | 60 | 32.4 | 78 | 42.2 | 32 | 17.3 |
| Change in attitude towards basic sciences and role of these in medical practice |
23 | 12.4 | 36 | 19.5 | 76 | 41.1 | 50 | 27.0 |
table.5. students attitude towards the program (Polar questions) n=185
| S.No. | Polar questions | Yes | No |
| 1 | Percentage of students who opined that the program helped them to understand the concepts better |
156(84.3%) | 29(15.7%) |
| 2 | Whether the program motivated them to study basic science subjects. |
145(78.4%) | 40(21.6%) |
| 3 | Need of including the program in 1st MBBS curriculum | 173(93.5%) | 12(6.5%) |
was involved, 78.4% (n=145) felt that the program increased their motivation to study basic science subjects and 93.5% (n=173) agreed that it is essential to include the present kind of program in 1st MBBS curriculum (Table. 5).
Discussion
In the present setup of the undergraduate medical curriculum, students are exposed to clinical subjects only from the second year. However, it has been observed that students find it difficult to recollect essential basic concepts during their clinical postings.15 The goals of medical education should be student oriented in which the development of the student should progress along with knowledge, skills and attitude. Learning is an active process going on inside the student’s mind and teacher’s main role is to facilitate this learning process.16
It is now becoming more commonly recognized that the traditional structure of medical education created a large gap between the preclinical basic sciences years and the clinical postings in the later years of MBBS.
ECE is a teaching learning methodology, which fosters exposure of the medical students to the patients as early as the first year of medical college.17 The goals of ECE are to provide social relevance and context to basic science teaching and learning, enhance medical knowledge, learn few basic clinical skills and acquire a wide range of attitudes.17
Integrated teaching inter-relates or unifies subjects frequently taught in separate academic courses or departments.18 Integrated learning refers to when knowledge and skills from across the disciplines are called upon to address patient cases, problems and issues, to create learning experiences for students. Thus an “integrated medical curriculum helps graduates to put together the learned facts so as to get the whole picture and adopt a holistic approach while treating a patient.19
ECE and Integrated teaching-learning are two of the curricular reforms recommended by the MCI to be introduced in the first year of undergraduate medical studies to have a holistic approach instead of a fragmented learning and bridge the gap between the preclinical and clinical years of MBBS.17
In the present study an attempt was made to implement a program which exposed the first year MBBS students to clinical cases and also integrate their knowledge on all the three aspects i.e anatomical, physiological and biochemical aspects of the clinical cases.
Students opined that early clinical exposure with horizontal integration has helped understanding the basic subjects to a significant to great extent (79.4%), helped in understanding the concepts better, compared to the other topics where only traditional teaching was involved(84.3%), the findings similar to previous studies.20,21 The components of the program which helped them in understanding the subject better were case based seminars, examining and interacting with the patients, horizontal integration of the learning process and the team work as they worked in groups in preparing for the seminar presentations. It is clear that the program has significantly contributed towards developing interest in the subject, improved their communication skills, and helped them to integrate the knowledge in the topics covered, the finding consistent with a study done in a medical college in Maharashtra.22 The results of our study suggested that the program has contributed towards developing sensitivity towards patient problems and needs to a significant to great extent (61.6%) which is consistent with the findings of other studies.15,20,23 ECE can play a significant role in changing the student’s attitude towards basic sciences subjects and to understand their role in medical practice. Majority (78.4%) of the students opined that the program contributed towards motivating them to study the basic science subjects, a finding consistent with previous studies.24,25 93.5% of the students felt that it is essential to implement the present program as one of the teaching learning methodologies in the curriculum, a finding consistent with a study done by Solomon Satish Kumar et. al.20
ECE and Integrated learning can be used as effective tools to enlighten the scope of medical sciences for beginners and emphasizing the importance of basic sciences in patient care. Traditionally students often spend long hours in the classroom listening to didactic lectures. So these programs help in empowering the students to become efficient physicians.26
In view of the good/excellent rating (90.2%) of the program by the students, it is being planned to implement the program in teaching basic science subjects for future groups of students, incorporating their suggestions. An objective analysis of the effectiveness of this approach can be made by comparing student's performance with and without the program.
Conclusion
From the present study, it can be concluded that implementation of programs like early clinical exposure and integration of the subjects can make learning basic science subjects more interesting and can affect the student’s attitude towards patient care when compared to traditional teaching for medical students. As it is difficult to include all the topics of basic sciences in this program it can be said that these programs cannot completely replace the traditional didactic lectures but they can definitely help in reinforcing didactic lectures. The program needs extra efforts from the faculty and they may require some level of training before implementation of such programs. Coordination between the preclinical and clinical departments is a prerequisite for proper implementation of the program.
Acknowledgement
The authors thank our colleagues from the departments of Anatomy, Physiology and the concerned clinical departments for their immense contribution in smooth conduction of the program. Authors also acknowledge the immense help received from the scholars whose articles are cited and included in the references of this manuscript. The authors are also grateful to the students of 1st year MBBS for their active participation and cooperation.
References
- Bligh J: Learning about science is still important. Med Educ. 2003, 37 (11): 944-945. 10.1046/j.1365-2923.2003.01703.x.
- Custers EJFM: Long-term retention of basic science knowledge: a review study. Adv Health Sci Educ Theory Pract. 2010, 15 (1): 109-128. 10.1007/s10459-008-9101-y.
- Lazic E, Dujmovic J, Hren D: Retention of basic sciences knowledge at clinical years of medical curriculum. Croat Med J. 2006, 47 (6): 882-887.
- Norman G: The essential role of basic science in medical education: the perspective from psychology. Clin Invest Med. 2000, 23 (1): 47-51.
- Gonnella JS, Hojat M, Erdmann JB, Veloski JJ: Assessment measures in medical school, residency, and practice: the connections. 1993, New York: Springer
- Pritha.S.Bhuiyan, Nirmala N.Rege, Avinash Supe. The art of teaching medical students, 3rd edition, ELSEVIER publications, 2015, chapter 10, page no. 124-125.
- Littlewood S, Ypinazar V, Margolis SA, Scherpbier A, Spencer J, Dornan T. Early practical experience and the social responsiveness of clinical education: systematic review. BMJ. 2005; 331:387-91.
- Dahle L, Brynhildsen J, Berbohm FM,Rundquist I, Hammar M. Pros and cons of vertical integration between clinical medicine and basic science within a problem- based undergraduate medical curriculum: examples and experiences from Linkoping, Sweden. Med Teach. 2002; 24:280-5.
- Kate MS, Kulkarni UJ, Supe A, Deshmukh YA. Introducing integrated teaching in undergraduate medical curriculum. Int J Pharma Sci Research 2010; 1(1): 18-22.
- Joglekar S, Bhuiyan PS and Kishore S. Integrated teaching- our experience. J Postgrad Medicine 1994; 40(4): 231-232. Huber MT, Hutchings P. ‘Integrative learning. Mapping the terrain’. Association of American colleges and Universities and the Carnegie Foundation for the advancement of Teaching. 2004; 1-18.
- Bhuiyan PS, Rege NN, Supe AN. The art of teaching medical students. Medical Education Technology cell, Seth G.S. Medical College and K.E.M Hospital, Mumbai. 2nd ed. 2002 ; 305-312
- Vision 2015, Medical Council of India. Published by Medical Council of India, Year of Publication: March 2011, Available from http://www.mciindia.org/tools/ announcement/MCI_booklet.pdf)
- Shimura T, Takumi A, Shimizu K et al. Implementation of integrated medical curriculum in Japanese medical school. J Nippo Med Sch 2004; 71: 11-16.
- Ebrahimi S, Kojuri J, Ashkani-Esfahani S; Early clinical experience: A way for preparing students for clinical setting. GMJ, 2012; 1(2): 42-47.
- Tayade MC , Kulkarni NB , The Interface of Technology and Medical Education in India: Current Trends , Indian Journal of Basic & Applied Medical Research; December 2011: Issue-1, Vol.-1, P. 8-12
- Kachur EK. Observation during early clinical exposure- an effective instruction tool or a bore. Med Educ 2003, 37:88-89.
- Harden RM, Sowden S, Dunn WR. Some educational strategies in curriculum development: The SPICES model. ASME Medical Education Booklet number 18. Med Educ 1984,18:284–97.
- Malik AS, Malik RH. Twelve tips for developing an integrated curriculum. Med Teach 2011, 33:99-104.
- Solomon Sathish kumar, Nihal Thomas, Elizabeth Tharion, Nithya Neelakantan and Rashmi Vyas. Attitude of medical students towards Early Clinical Exposure in learning endocrine physiology, BMC Medical Education, BMC series open, inclusive and trusted 20077:30. DOI: 10.1186/1472-6920-7-30, ©Sathishkumar et al; licensee BioMed Central Ltd. 2007
- Lalita Harish Nikam, Sneha Vitthal Chopade. Introduction Of Horizontal Integration And Comparison With Traditional Teaching Methods In Physiology, Ijbms, International Journal Of Basic Medical Science, Volume:6, Issue:1, 2015 April, Issn-0976-3554
- Suresh Chari, Madhur Gupta and Shubhda Gade. The Early Clinical Exposure Experience Motivates First Year MBBS Students: A Study, Int J Edu Sci, 8(2): 403-405 (2015) © Kamla-Raj 2015
- Bita Afra, Mahasti Alizadeh*, Simin Taghavi, Hossein Jabbari Bayrami, Javaher Yari, Res Dev5.The Impact of Early Clinical Exposure on the Knowledge and Attitude of Basic Sciences Medical Students at Tabriz University of Medical Sciences. Med Educ, 2015, 4(1), 55-60 doi:10.15171/rdme.2015.009, http://journals.tbzmed. ac.ir/rdme
- Alka Rawekar, Arunita Jagzape, Tripti Srivastava, and Shashank Gotarkar. Skill Learning Through Early Clinical Exposure: An Experience of Indian Medical School, J Clin Diagn Res. 2016 Jan; 10(1): JC01–JC04. Published online 2016 Jan 1. doi: 10.7860/ JCDR/2016/17101.7022)
- Baheti SN, Maheshgauri D. Early Clinical Microexposure (Ecmix) (A Path From Early Clinical Micro Exposure to Early Clinical Macro Exposure (Ecmax) Global Journal For Research Analysis. 2015;4(3):1–2.


